Eating disorders can be difficult, but they become even more difficult when a co-occurring mental health condition is present. With over 30 million men and women developing an eating disorder at some point in their lives, it is not uncommon that they would also battle a dual diagnosis. The prevalence of a co-occurring mental health condition with an eating disorder makes addressing both conditions during treatment vital.
What are the common co-occurring mental health disorders?
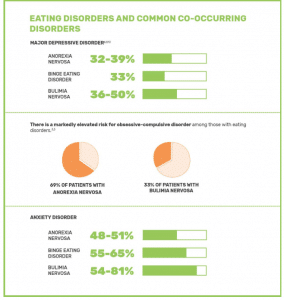
Depression, anxiety, or obsessive-compulsive disorder are the most common mental health conditions to co-occur with an eating disorder.
Depression affects just over 322 million across the globe. In the US, over 15.7 million people ages 18 older have experienced at least one major depressive episode in the past year. A depressive disorder can cause intense feelings of sadness that occupy the mind endlessly and interferes with daily activities. Symptoms of low energy levels, low self-esteem, and fluctuations in appetite and weight can all play a role in an eating disorder.
Anxiety is the most common form of mental illness, affecting an estimated 264 million people globally. Over 19% of US adults had an anxiety disorder in the past year. We all experience normal anxiety and stress, but when it begins to interfere with daily life, it could be the sign of an anxiety disorder. Eating disorders are often used as a coping method for intense anxiety.
Obsessive-Compulsive Disorder (OCD) is an anxiety disorder and the most common to co-occur with an eating disorder. Although they recognize it is not rational, over 1.2% of US adults experience obsessions and compulsions related to OCD. Those who have OCD and an eating disorder will often develop compulsive food rituals and obsessive thoughts about food.
Why does a dual diagnosis occur?
No one can say with 100% certainty why the link between eating disorders and mental health disorder exists, but they are clearly interwoven. A mental disorder can begin around the same time as an eating disorder or after the eating disorder behavior has begun. Sometimes the depression, anxiety, or OCD may be a result of the eating disorder behaviors. Restricting calories, binging, and purging can all take a toll on the mental health of an individual. Some mental health conditions can also be a risk factor in someone developing an eating disorder, as the eating disorder may develop as coping mechanisms for many of these conditions.
When looking at some of the most common eating disorders, we can see there is a clear connection.
Anorexia frequently co-occurs with a mental health condition, with studies showing over 56% of those with anorexia having at least one other mental disorder. One study found that over a third of those with an anorexia diagnosis also have major depressive disorder. Additionally, almost 50% have some form of anxiety disorder, including obsessive-compulsive disorder and social phobia. Many individuals with anorexia show signs of anxiety years before their eating disorder symptoms are present. Anxiety can cause people with anorexia to feel a false sense of control by using food, weight, and exercise.
Bulimia is more prevalent than anorexia and nearly half of those battling this disorder have some type of a mood disorder, and more than half have anxiety. Additionally, a third of those with bulimia suffer from OCD. Individuals with bulimia often find their sense of self-worth dependent on their body size and shape. The inability to achieve the desired body image will often contribute to depression.
Binge Eating Disorder is the most common eating disorder is the US, and just over 79% of those with the disorder also have a co-occurring mental health condition. Over half of those with binge eating disorder have some form of anxiety disorder. The inability to control their food intake will often lead individuals to have increased anxiety.
How do you treat dual diagnosis?
Treating both the eating disorder and mental health disorder is a key part of successful recovery. At the Toledo Center for Eating Disorders, we understand this and the need to tailor a specialized plan that meets these unique needs and is tied into the therapeutic healing process.
Meggan Desmond, Clinical Director at Toledo Center shares, “It is important to understand the relationship and influence between theses multiple conditions and how they affect one another. Our treatment goals are designed to address the underlying issues and co-occurring conditions that exist with the eating disorder in order for people to have the best treatment outcome.”
We work with adult and adolescent males and females to ensure they understand all aspects of their eating disorder and co-occurring mental health condition and provide the treatment needed for sustainable recovery. Using evidence-based therapies that incorporate elements of mindfulness, positive psychology, nutritional rehabilitation, and psychotherapy , we help clients identify the underlying issues that are contributing to their eating disorder. As clients begin to understand these problems and challenge their cognitive distortions, they can identify and practice new coping skills.
We know that seeking help for an eating disorder requires strength and courage. At Toledo Center, we provide the support and guidance needed that makes full recovery possible. Call our admissions team today or complete our contact form for more information.

